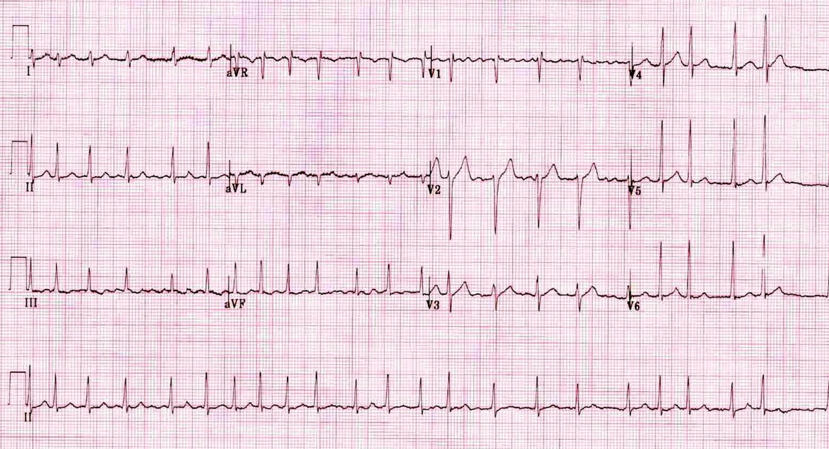
EKG #1
What’s the rhythm?
EKG #2
Dude, what’s the rhythm?
EKG #3
Home skillet, what’s the rhythm?
BONUS QUESTION: What is a Lewis Lead?
EKG #1 - Atrial Fibrillation
· Super irregular! This is probably the most common irregularly irregular rhythm we see
· You may have confused this with atrial flutter because of the coarse fib waves in V1
o First, you’re not alone: 1999 study showed high frequency of incorrect diagnosis, even by cardiologists: https://www.ncbi.nlm.nih.gov/pubmed/10549907
o It may not matter, since aflutter and afib are treated same way in the ED
But since you’re all nerds like me, here’s how to differentiate…
1. The waves in atrial flutter are much more uniform than the ones above.
2. Flutter waves are classically sawtooth morphology
3. Remember atrial flutter can be regular. It is only irregular when you have variable conduction.
I.e. when you have two flutter waves and a QRS, then three flutter waves and a QRS, then four, then two again…
EKG #2 - Multifocal Atrial Tachycardia (MAT)
· Multiple foci in the atria triggering the AV node. Look at all the different P wave shapes!
· Three separate P wave morphologies = diagnostic of MAT
· The slow version of MAT is a wandering pacemaker (MAT without the T)
· Classically presents in a patient with COPD or CHF
· Note that this EKG has R axis deviation, perhaps from cor pulmonale
EKG #3 - Premature Atrial Contractions, Normal Sinus Rhythm
· So this is yet another irregularly irregular EKG, and at first glance you may call this atrial fibrillation.
· However, note all the well defined p waves – this is sinus tach
· So why is it irregular?
· Before those irregularly occurring QRS complexes, there is a p wave, and it looks exactly the same as all the other p waves (in height, width, and axis)
· The SA node is firing early, depolarizing the ventricles, and creating an irregular rhythm
What is a Lewis Lead?
Ohmygod, great question, so glad you asked!
From Wikipedia: “A Lewis Lead is a modified ECG lead used to detect atrial [activity] when [it] is suspected… but is not definitively demonstrated on the standard 12 lead ECG.”
So you think someone has atrial flutter (sustained HR of 145 perhaps?) but you can’t see any p waves or sawtooth activity.
Maybe you’re trying to discern SVT from fast sinus tach?
How can you solve this conundrum?
Lewis Lead!
1. You can do this on the monitor, you don’t need a 12lead
2. Arrange the leads as seen here. (The green one can go anywhere, it’s just an electrical ground)
3. Check for atrial activity
Before the Lewis Lead… (where the p waves at?)
After the Lewis Lead! (Retrograde p waves, mostly upright at the end of the QRS. No p waves prior to the QRS. This is SVT.)
Lewis Lead
https://en.wikipedia.org/wiki/Lewis_lead
http://hqmeded-ecg.blogspot.com/2018/03/hypotensive-and-tachycardic-in-clinic.html
Long article about atrial fibrillation:
http://www.emdocs.net/more-atrial-fibrillation-management-pearls-in-the-ed/
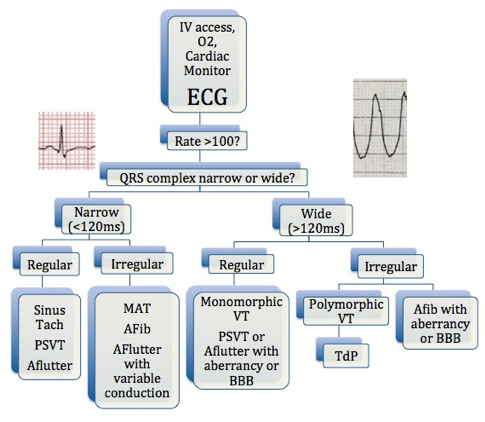
You need to memorize this flow chart! (Courtesy of ALiEM)
Tachydysrhythmia Algorithm