I think we all dread this: Just imagine this scenario: you are concerned that your patient has a pulmonary embolus. They are tachycardic, hypoxic on room air, but BP’s are stable (for now). They were a tough stick and 2 nurses tried for 5 minutes, so under real time ultrasound guidance you place what you think is an expert 20g x 48mm angiocath in their right cephalic vein.
You dial 6308 and ask the radiology technologist to scan the patient next, then you are off to see the next patient on a busy north side shift.
15 minutes later, you get a call: “Ummmm… Doc, patient x…. that line blew. They got the hole load in the right arm. Can you come take a look?”
This can happen about 0.24% of patients who receive IV contrast in the upper extremity (or about 1/400 studies).
UNDERSTANDING CONTRAST:
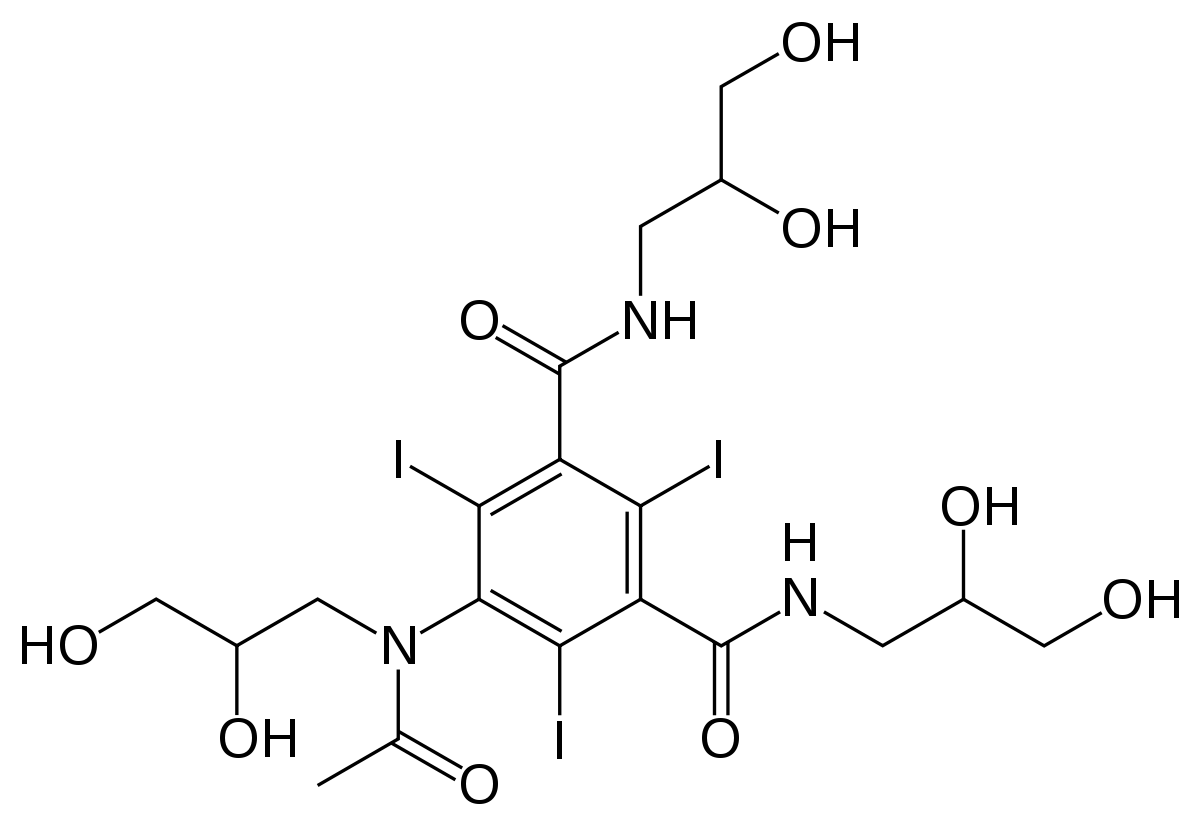
The Omnipaque™ we use for our IV contrast CT studies is Iohexol:
Here is its structure:
The concentration we use is 350 mg/mL, this results in a total osmolality of 844 mOsm/kg water. This is approximately 3 times the osmolality of serum. However, given the fact it is non-ionic, it does not cause a significant osmolar effect. Nonetheless, infiltration will lead to fluid shift of H2O down its gradient into the tissue compartment the infiltrated contrast material occupies, which is typically the interstitial space. This has been shown experimentally in a renal model: after contrast load urine output increases because the iohexol is renally excreted.
The most danger for infiltration occurs with high flow rates achieved during CT angiography studies. As per our technologist on our Siemens machine, the auto injector we use has a flow rate 4-5 mL/s achieved with a pressure gradient anywhere from 50-100 psi. If the IV has poor flow due high intracatheter or intravenous resistance, then the pressure can increase to upward of 400 PSI to achieve flow. When this high pressure occurs, the IV can become dislodged. Remember Newtonian mechanics: Pressure exerts a force, and for each force there is an equal and opposite reaction.
MANAGEMENT OF IV INFILTRATION OF A CONTRAST LOAD:
####first and foremost, you need to inform the patient what happened. Explain why this happened. Apologize for the complication. Address any pain issues. Tell them how you and the team will care for their likely painful upper extremity. Finally, you can reassure them for the reasons below.
*Gradually, the infiltrated contrast will diffuse out of the tissue compartment and back into the serum. This diffusion can be enhanced with gentle warm compresses.
**Plastic surgery recommendations for this complication are elevation of the extremity, local massage, and frequent neuromuscular checks.
***In a study of 102 cases of IV contrast extravasation in the upper extermity, surgical intervention was required in 0. The surgeons behind this study recommend surgical consultation if there obvious signs of skin compromise or compartment syndrome.
****compartment syndrome has been reported in the case literature, so please, please, please, watch for that. The incidence is on case report level, so it is likely very, very low.
SOME TIPS PREVENTION OF IV INFILTRATION OF US GUIDED PIV’s:
*Always use the 48 mm angiocath
**The more of the catheter that is in the lumen of the vein, the less likely it is to become dislodged. So a good rule of thumb is at least 1 cm of the catheter within the lumen of the vein. So any target >2cm deep to the skin will be difficult to properly position using a 45 degree angle of approach.
One fun final fact: non-ionic iodinate contrast materials are procoagulants and as per the FDA they should be avoided at all cost patients with homocystinuria.
AS ALWAYS FEEDBACK IS ENCOURAGED.IF YOU HAVE AN INTERESTING QUESTION, FACTOID, OR OPINION, PLEASE RESPOND ALL.
Best regards,
Wells
References:
https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/018956s095,020608s031lbl.pdf
https://www.sigmaaldrich.com/catalog/substance/iohexol821146610895011?lang=en®ion=US
Jonas Pologe’s US PIV POD
Belzunegui T, Louis CJ, Torrededia L, Oteiza J. Extravasation of radiographic contrast material and compartment syndrome in the hand: a case report. Scand J Trauma Resusc Emerg Med. 2011;19:9.
Sbitany H, Koltz PF, Mays C, Girotto JA, Langstein HN. CT contrast extravasation in the upper extremity: strategies for management. Int J Surg. 2010;8(5):384-6.
Solomon R. Contrast media: are there differences in nephrotoxicity among contrast media?. Biomed Res Int. 2014;2014:934947.