To kick off the block I’ll be talking about hip dislocations as today is ~Trauma Tuesday~ after all. I have only attempted to reduce one hip myself and it was while I was at Midwood Community hospital a few weeks ago. Dr. Duo Xu and I were pushing and pulling with all our might but despite all our best efforts, ultimately it was unsuccessful and the patient was transferred to MMC main for orthopedics. Honestly, we were not surprised as the patient had dislocated it the prior day and also had a hip replacement. This inspired me to want to delve into this topic some more, especially on reduction techniques.
Classifications
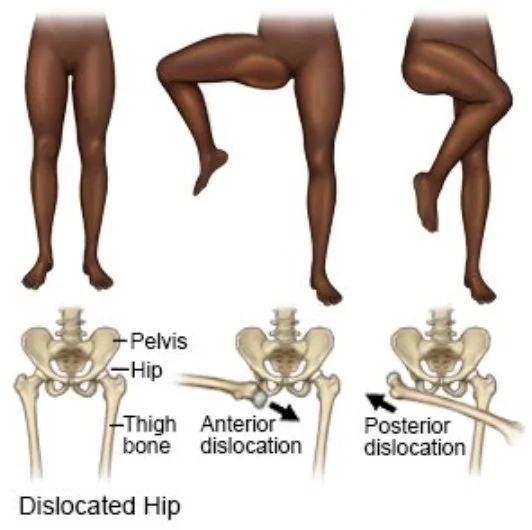
Posterior: Most common, 90% of hip dislocations
Occurs when an axial load is applied on a Flexed and ADDducted hip
ie motor vehicle crashes where patient's knee hits the dashboard
Anterior: 10% of hip dislocations
Occurs when an axial load is applied on a Extended and ABducted hip
As with other dislocations, you always want to be mindful of injury to the nearby vessels and nerves. Depending on the mechanism of injury, there may be an underlying fracture. If there is an associated fracture, this becomes a complex dislocation.
Management for simple closed isolated hip dislocation
Obtain xray films, pain medication
Reduce ideally under 6 hours to reduce chances of developing avascular necrosis. One study found that after 6hrs, 53% of patients developed avascular necrosis
Procedural sedation
Management for complex closed isolated hip dislocation
If there is an associated femoral fracture then you’ll need to get orthopedics on board. They may take the patient to the OR and have everything taken care of intra-operatively.
Reduction techniques
There are dozens of methods and various combinations/modifications but I'm going over a few that I think are more intuitive and less likely to injure myself.
Rocket Launcher
Patient supine in stretcher almost with both legs hanging off stretcher
You flex their knee and facing their feet, put your shoulder underneath the posterior fossa/calf with hands around lower tibia/ankle
Use your shoulder to press upwards while hands pull down
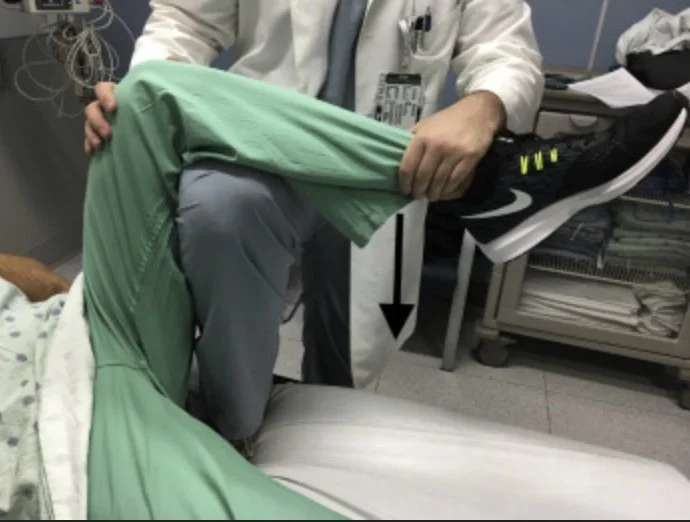
Captain Morgan
Patient supine in stretcher
You have one leg flexed on stretcher and other leg flat on ground with patient’s calf on your thigh
Push down by patient’s ankle, can also plantarflex your foot that’s on the stretcher to get more leverage
For short kings and queens a step stool may be helpful, I could barely get my foot comfortably up on the stretcher without feeling like I was about to dislocate my own hip
Allis
Patient supine in stretcher
You put your hands around ipsilateral tibia, standing on stretcher can get you better leverage
Pull upwards, remember that consistent traction is key
Some personal takeaways
Don’t forget you need a nurse to record vitals / draw meds during the procedural sedation and during that time you are utilizing a lot of resources.
You need at least one assistant to help keep the pelvis in place while you are reducing for all these maneuvers shown above
Maximizing pain relief and relaxation will increase your chances of success, your patient should be loosey goosey. Consider a regional nerve block (femoral, fascia iliaca)
Dislocated hardware joints are extremely difficult to reduce, once I had three orthopedic residents yanking on a dislocated hip while the EM attending and I helped pull traction
You may wake up sore the next day
References: