When and when not to perform paracentesis? Think of the indications for emergent paracentesis in a similar fashion to emergent thoracostomy. Indications:
Relief of respiratory distress caused by massive ascites
Diagnostic for infection ie. suspected spontaneous bacterial peritonitis
Contraindications?
Overlying cellullitis
Vasculature or bowel obstructing desired site
Loculated fluid (concern this may be oncologic)
Significant coagulopathy INR < 8 platelets >20
2 minute EMRAP video outlining the procedure- https://youtu.be/9npNQM8ANds
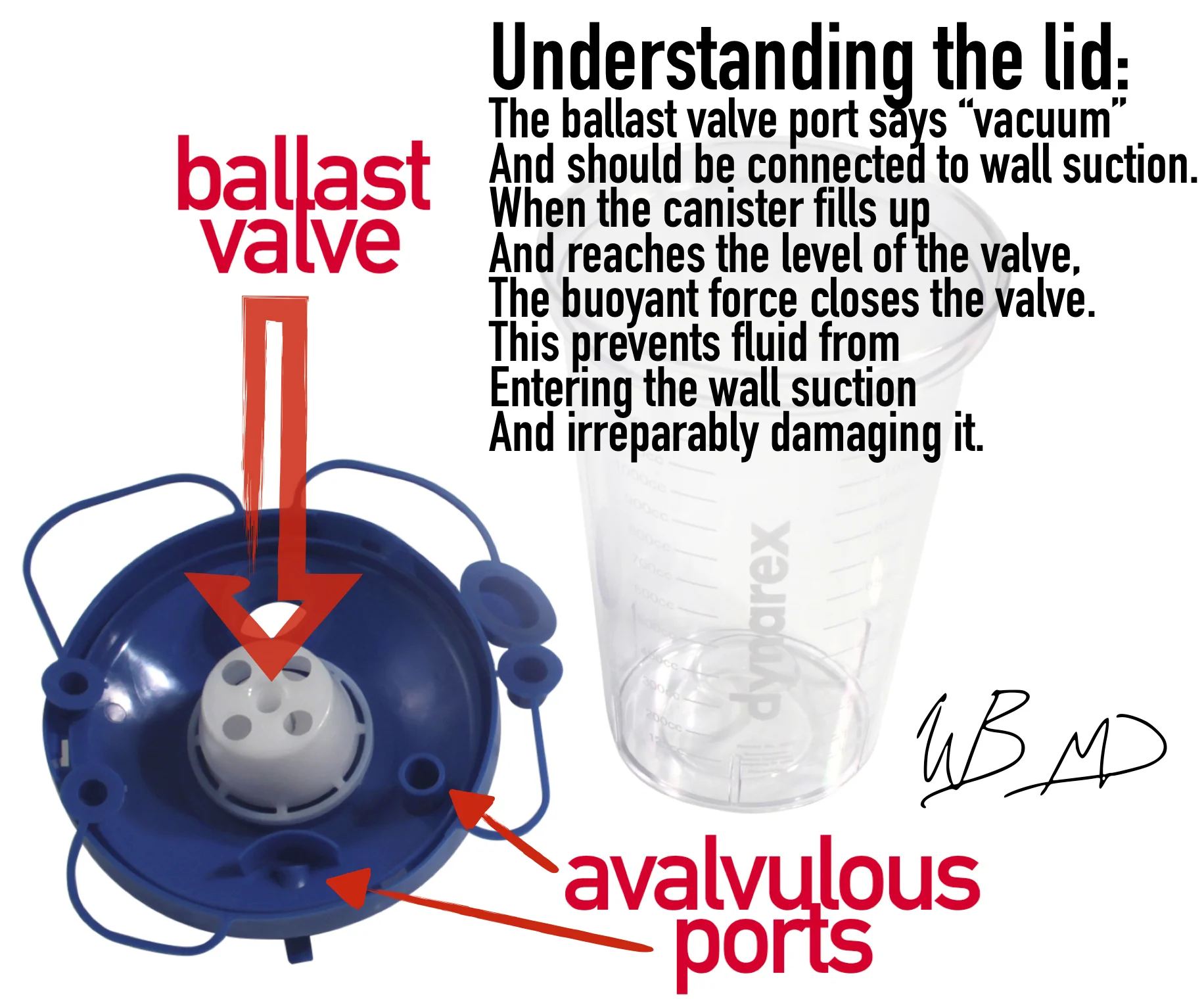
Blog post explaining in-series suction canisters- http://mmcedrco.w02.wh-2.com/EMBlog/suction-cannisters-in-series/