Disposition of Atrial Fibrillation For other pearls of the day regarding afib, follow the links here: Rhythm Control and Cardioversion Holiday Heart Syndrome Ottawa Aggressive Protocol
Admit - indications: hyperthyroidism, ischemia, infectious process, CHF, difficulty with rate control - ablation therapy indications: difficulty with controlling ventricular rate, LV dysfunction, rate-related cardiomyopathy, refractory symptomatic paroxysmal afib
Discharge - stable patients may be discharged with outpatient follow up if rate-controlled and absence of structural heart disease - if required medications for rate control during ED stay, prescribe same class of medications when discharged (e.g., metoprolol tartrate 50 mg PO BID or dilitiazem ER 120 mg or 180 mg PO daily) - risk of stroke is equal for paroxysmal and persistent afib, and so anticoagulation should always be considered based on CHA2DS2VASc score
CHA2DS2VASc Score - congestive heart failure - hypertension - age > 74 (2 points) - diabetes - previous TIA/CVA (2 points) - vascular diseases (e.g., CAD, MI, PVD) - age 65 - 74 - female - score 0 = low risk - score 1 = low-moderate risk (consider antiplatelet or anticoagulation) - score 2 = moderate-high risk (anticoagulation indicated) - consider bleeding risk for patients prior to starting (ATRIA Bleeding Risk Score)
Anticoagulation - oral anticoagulation preferred: apixaban, dabigatran, rivaroxaban, warfarin - patients not suitable for anticoagulation (if not due to risk of bleed) -> clopidogrel and ASA (81 mg - 325 mg) - afib + mitral stenosis -> warfarin - afib + stable CAD -> warfarin - afib > 48h -> warfarin OR heparin OR dabigatran for at least 3 weeks prior to cardioversion
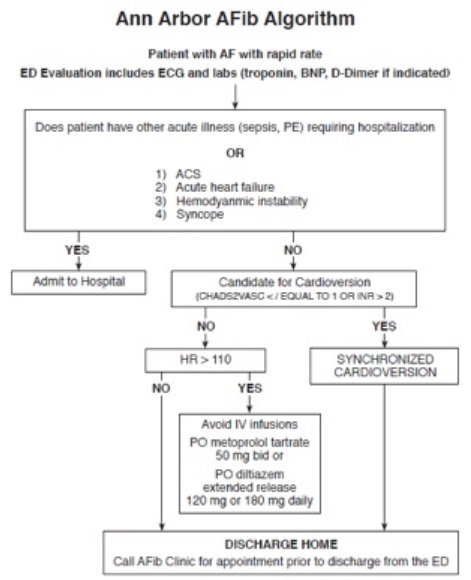
Resources LITFL, Atrial Fibrillation: https://lifeinthefastlane.com/ccc/atrial-fibrillation/ Anticoagulation Dosing: http://www.acc.org/tools-and-practice-support/clinical-toolkits/atrial-fibrillation-afib/anticoagulant-dosing-table Emergency Medicine Cases: https://emergencymedicinecases.com/episode-20-atrial-fibrillation/ Ann Arbor Afib Algorithm: https://www.acep.org/_QIPS-Section-Microsite/Improving-and-Standardizing-Care-of-Patients-with-Atrial-Fibrillation-in-a-Community-Emergency-Department/#sm.0000o9mbwcinmefstkr1zrovyb3vu
