>> Why do we care?
Results in inability to ventilate (massive loss of TV necessitating ETT replacement)
Results in aspiration of gastric contents or pharyngeal secretions (no proper isolation to protect the lungs)
Can result in complete loss of airway
>> How does it present?
Respiratory instability (decreased oxygenation and/or ventilation)
Gurgling noise
Decreased tidal volumes
>> Two Major Categories:
Leaks Around an Intact Cuff/Inflation System:
Cuff Underinflation
Cephalad Migration of ETT
Inadvertent Intratracheal Placement of Gastric Tube
Discrepancy Between ETT and Tracheal Diameter
High Mean Airway Pressure
Leaks Due to a Defective Cuff and/or Inflation System:
Inflation Valve: Can be incompetent as a result of poor manufacturing, mechanical trauma, or even routine connection of syringe
Pilot Tubing: May be damaged by tube securing devices, accidentally cut, or manufactured poorly
Pilot Balloon: Can be torn, punctured, or otherwise damaged on teeth or sharp equipment; this can cause leakage of air or failure to inflate altogether
ETT Cuff: If this occurs, the tube must be changed!
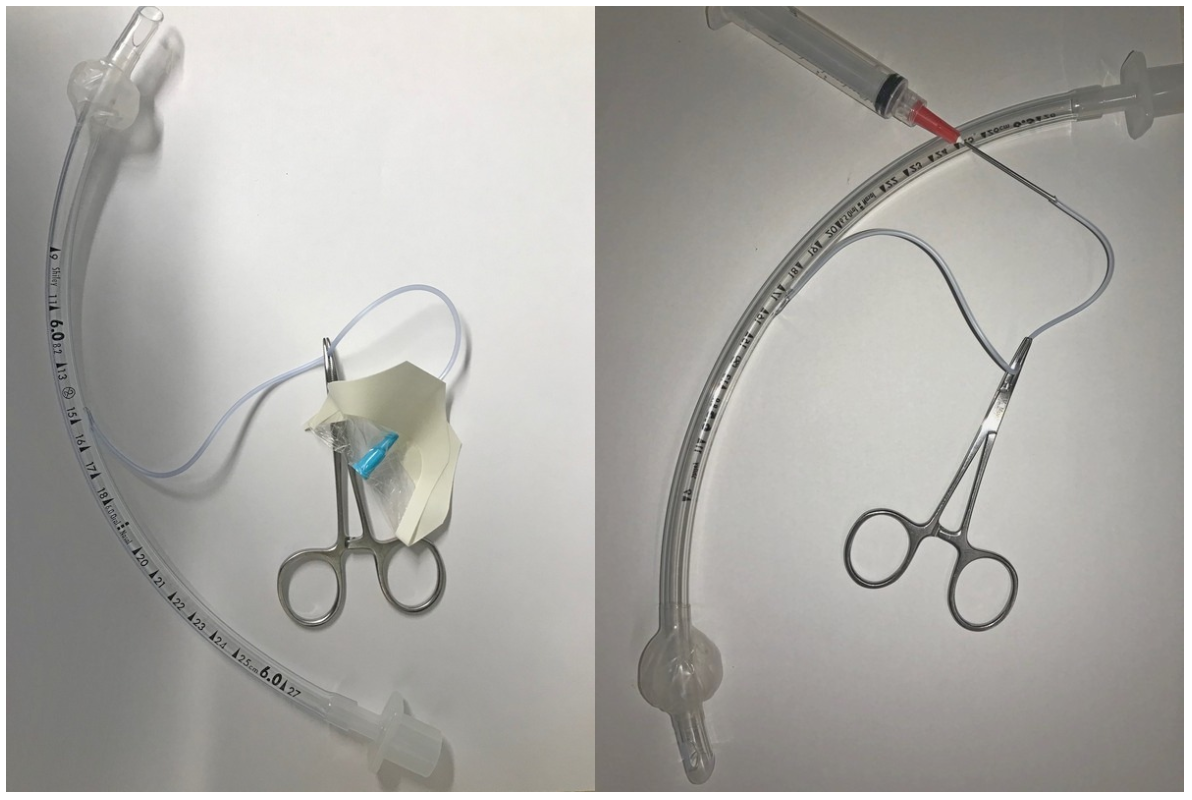
Situation 1: The one-way valve malfunctions, but the pilot balloon and line are intact.
Attach a T-piece connector or a clave to the pilot balloon, and then inflate with a syringe. Clamp the T piece with a hemostat or IV tubing clamp, and disconnect the syringe
Situation 2: The pilot balloon or pilot line is ruptured.
Cut the line below the break. Insert either a blunt needle or a 22G catheter into the lumen of the line. Connect it to a syringe and inflate the cuff. Clamp the line, and cover needle or catheter with a transparent film dressing or clave.