Electrical Storm
Background
three or more episodes of sustained ventricular tachycardia, ventricular fibrillation, or appropriate ICD shocks in a 24 hour period
frequently, hemodynamic unstable
believed to mostly be due to catecholamine surge (sympathetic overdrive), but need to consider the causes below:
MI
Electrolytes
Acute HF
QT prolongation/shortening
Torsades
Brugada
Thyroid storm
Drugs
Sepsis
Presentation is broad
May complain of pain from ICD shocks, palpitations, syncope
Can present in cardiac arrest
Management
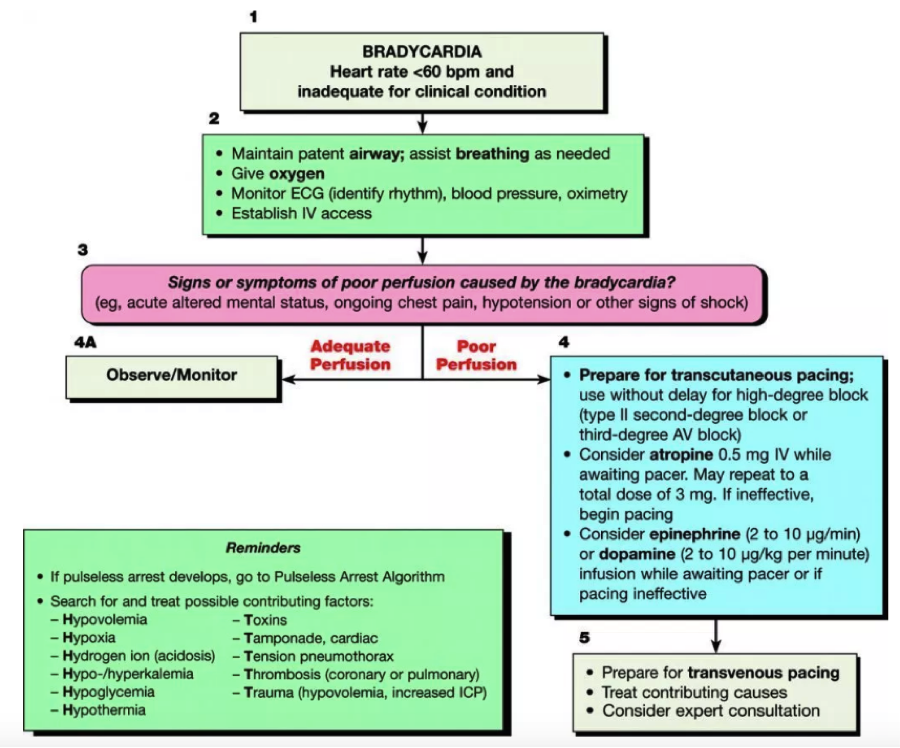
ABCs
ACLS guidelines should be followed
Pulse (VT)==>cardiovert
Pulseless (VT/VF)==>defibrillate
Consider dual defibrillation if VT/VF persists after 5 delivered shocks (see image below)
Coordinate firing of both defibrillators at the same time
Should you place a magnet over ICD if patient has one?
Remember, magnets turn of the ability to defibrillate, but don't affect pacing capability
If you want the patient to be shocked then do not place a magnet, unless you think you’re dealing with something other than VF/VT and thus it is shocking inappropriately (sinus tach, afib)
Practice variation exists. Some will place the magnet, especially if the pt is stable, to spare pt more anxiety/pain contributing to the storm
Start them on an anti-arrhythmic
Amiodarone 300mgè150mg IV //
Procainamide 10 mg/kg IV over 20 min //
Lidocane 1-1.5mg/kg IV
Add a Beta Blocker to suppress the sympathetic tone and increase the dysrhythmia threshold
Metoprolol 2.5-5mg IV q2-5min //
Propranolol .15mg/kg IV over 10 min followed by standing order//
Esmolol 300-500 mcg/kg push followed by drip
Consider an anxiolytic or sedation
Brugada
Unlike aforementioned, VF in these pts is thought to be due to excessive vagal tone
Isoproterenol drip will increase the sympathetic tone
Quinidine has been shown to help
Torsades
Magnesium, replete electrolytes
If have episodes of bradycardia then add isoproterenol drip
Dispo
Admit to CCU if possible
May need cath lab, ablation, ECMO