POTD: Idiopathic intracranial hypertension
Idiopathic intracranial hypertension (IIH) aka pseudotumor cerebri and benign intracranial hypertension
· rare condition
· presents with gradual onset and chronic headache, vision changes, nausea, vomiting, and tinnitus
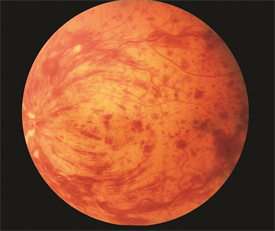
· + papilledema/ swelling of the optic disc on fundoscopy
· optic sonography
ONSDs should be measured 3 mm behind the papilla, an average of less than 5 mm is considered normal.
ONSD > 5 mm has been shown to be 90% sensitive and 85% specific for ICP > 20.
· Classic presentation: young, obese female
· + association has been found with this diagnosis and the use of oral contraceptive medications, tetracycline, anabolic steroids, and vitamin A
· Pathophysiology is not well understood but thought to be caused by an imbalance in CSF production and reabsorption
· Diagnostic criteria include an alert patient with either a normal neurologic examination or findings consistent with papilledema, visual field defect, or an enlarged blind spot
· Definitive dx: Lumbar puncture
done in a recumbent position reveals an elevated CSF opening pressure of more than 20 mm Hg in an obese patient (normal being up less than 20 mm Hg).
normal CSF analysis.
· CT head may show “slit like” or normal ventricles without mass effect
· DDx: glaucoma, venous sinus thrombosis, ICH, IC mass.
· Treatment
Repeat LPs
Acetazolamide
Surgical shunt if severe and refractory
offending agents such as oral contraceptive medications should be discontinued.
· Permanent loss of vision can occur in up to 10% of patients, and higher if left untreated
Sources:
Dubourg J, Javouhey E, Geeraerts T, Messerer M, Kassai B. Ultrasonography of optic nerve sheath diameter for detection of raised intracranial pressure: a systematic review and meta-analysis. Intensive Care Med. 2011;37(7):1059-68. [pubmed]
Blaivas M, Theodoro D, Sierzenski PR. Elevated intracranial pressure detected by bedside emergency ultrasonography of the optic nerve sheath. Acad Emerg Med. 2003;10(4):376-81. [PDF]
Peer IX