With the turn of the weather and puffy jacket season in full throttle, let's review hypothermia. In this POTD, we're going to be focusing on primary (environmental) hypothermia, and not hypothermia due to secondary causes such as sepsis, hypothyroidism, metabolic derangements, or trauma.
Hypothermia is defined as core temperature < 35C
between 1991-2011, an average of 1,300 deaths/year in the US attributed to environmental hypothermia
At risk populations: elderly, lack of shelter, alcohol/drug abusers, frequent exposure (winter sports)
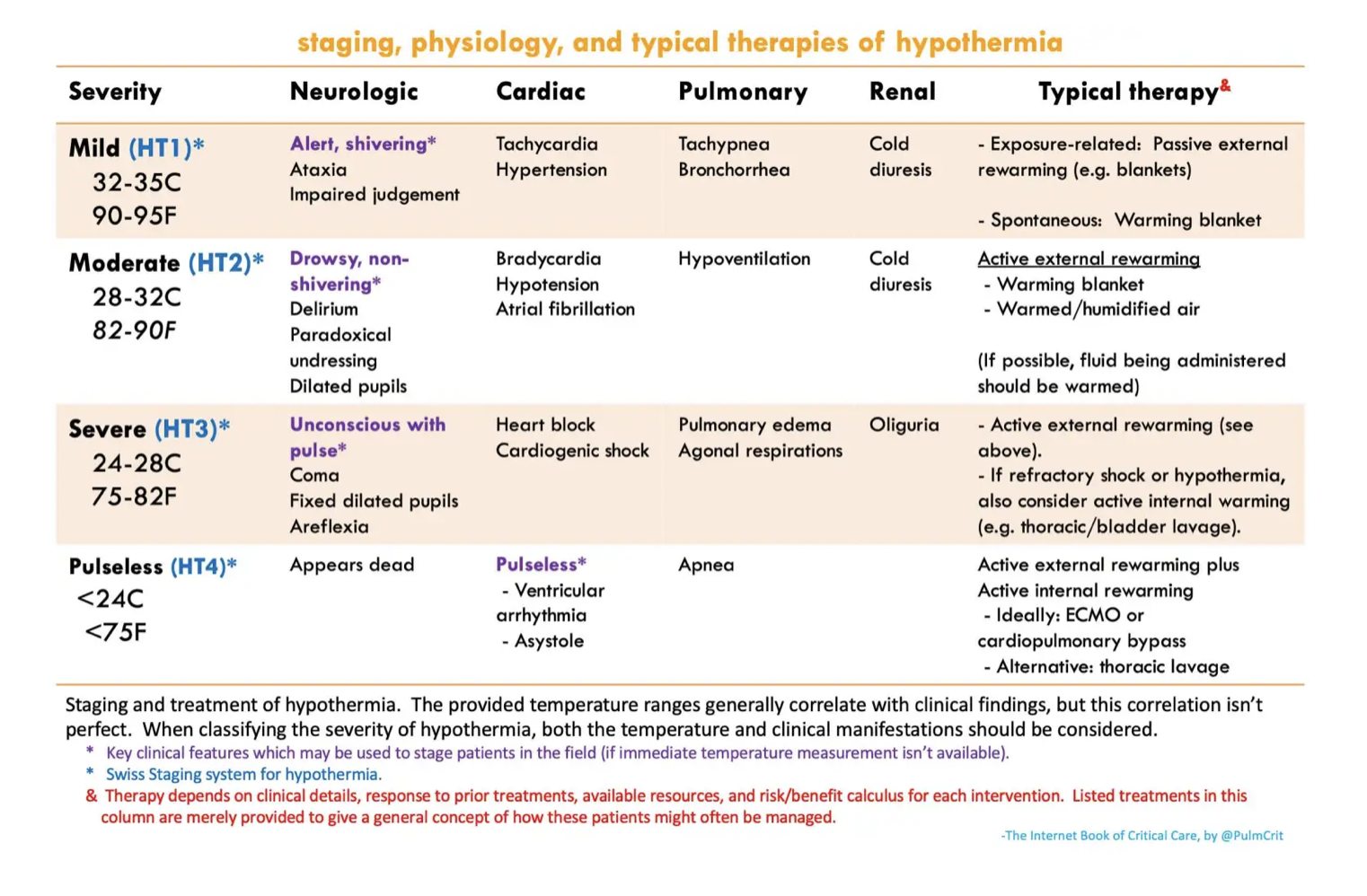
The modified staging system for hypothermia classifies severity into 4 categories, of which the chart below summarizes and demonstrates the general clinical picture
Initial evaluation should include the following:
Basic vital signs including core temperature
BGM (hypoglycemia)
EKG (bradycardia, Osborne waves, arrhythmias)
Basic labs (hypokalemia)
lactate, CK (rhabdomyolysis)
coags and fibrinogen (DIC)
consider TSH, cortisol,
Management of ABCs:
Airway/Breathing
Intubate as necessary, however encourage holding off intubation as patients are often hypotensive and prone to arrhythmias. Attempt rewarming and stabilization prior to hemodynamic stressors of intubation.
Circulation
bradycardia
hypothermia itself causes bradycardia, thus the key to treating bradycardia is rewarming. Giving medications to speed up HR is generally not encouraged and can induced arrhythmias
hypotension
again, often hypothermia induced, may also be secondary to bradycardia. Rewarming should improve pressures, and vasopressors generally discouraged as it can also induced arrhythmias
BUT - vasodilation can occur with rewarming, so if there is a drop in pressure, vasopressors should be considered
access
if central access is needed, keep the guidewire shallow to prevent entry into the right ventricle. The hypothermic heart is incredibly sensitive to VT/VF, so don't go tickling that ventricle. Femoral access or midline access is preferred
EKG in hypothermia:
Patient may initially present with tachycardia, however as hypothermia sets in, everything gets slower. Just imagine taking a NSR rhythm stripe and click-dragging it horizontally. You often see bradycardia, prolonged QTC, prolonged PR, and the presence of Osborne waves.
Osborne waves (also known as J waves) - a deflection at the junction of the QRS and ST segments, present usually temp < 30C. The size increases with worsening hypothermia
The most common dysrhythmia is atrial fibrillation, but cardiac arrest is due to eventual VF/VT or asystole
Management of hypothermia in the pulseless patient:
The famous phrase: "They aren't dead unless they're warm and dead" indeed is true. To be considered dead, the patient's core temperature should be ~32C before calling it.
ACLS: Modifications in setting of hypothermia
Delayed or intermittent CPR can be adequate due to low oxygen demand. Some say for T < 28, there can be pauses of <5 minutes CPR after every 5 minute interval of CPR if necessary.
Medications may fail to metabolize and will accumulate in the system, therefore prolonged intervals between epinephrine pushes and limiting repeated doses are recommended.
Similarly, defibrillation is poorly effective in T < 30C and repeated defibrillation may induce myocardial damage.
Suggested treatment by AHA: Can attempt one defibrillation if VF/VT present, otherwise hold further defibrillations and all IV medications until core T > 30C
Internal Rewarming:
ECMO: The best option for sever hypothermia. It allows for better organ perfusion, active rewarming as much as 7-10C per hour, and allows you to stop compressions. As an ECMO center, we should definitely consider getting ECMO downstairs to cannulate.
Thoracic Lavage: achieved through placement of two chest tubes, left preferred over right if only able to place one tube. Can achieve 3-6C warming/hour. Use Belmont or warm tap water if available, and monitor appropriate ins and outs to prevent tension PTX from improperly draining tubes
Bladder Lavage: less effective, however is easier to implement. Use dedicated 3-way Foley catheter or consider instilling 300 cc warmed fluids, hold for 15 minutes, and draining bladder. Rinse and repeat.
Management of hypothermia in patient with pulse:
External rewarming: Removing cold/frozen clothes and fully wipe down of snow. Employ external rewarming with Arctic Sun (preferred due to direct contact with skin to improve rewarming), warm blankets or Bair Hugger.
Respiratory rewarming: Warmth is typically lost through expirations. Therefore consider rewarming via respiratory support. In non-intubated patients, HFNC or CPAP/BIPAP with highest temperature settings. Intubated patients should have heated and humidified air set up with the ventilator (ask respiratory)
Fluid rewarming: hypothermia induced "cold diuresis," therefore patients often require volume resuscitation. Warm IV fluids, ideally crystalloid, should be administered. Keep in mind that this method prevents further dropping temperatures, but is ineffective for raising core temperature.
Lavage can also be considered in moderate/severe hypothermia in patients with pulses - see above.
Resources:
https://emcrit.org/ibcc/hypothermia/
http://www.emdocs.net/em3am-hypothermia-2/
https://www.saem.org/about-saem/academies-interest-groups-affiliates2/cdem/for-students/online-education/m4-curriculum/group-m4-environmental/hypothermia
https://wikem.org/wiki/Accidental_hypothermia