Why is baby aspirin 81mg instead of 80mg?
This is a remnant of the medieval apothecary system. In the late 1700s, medication dosages in the apothecary system were based on the weight of a grain of barleycorn, with the unit of weight termed the grain (abbreviated gr)1. The standard dose of aspirin used back then was 5 gr, equivalent to 325mg. This is also why Tylenol tablets also comes in multiples of 325mg. Baby aspirin was one quarter of that, which is equivalent to 81mg.
Where does the term “mad as a hatter” come from?
Poisoning. This comes from mercury poisoning. In the 18th and 19th centuries, mercury nitrate was used in the process of turning animal fur into felt products. Many hatters developed tremors and neuropsychiatric symptoms during this period2.
How glucagon received its name.
Kimball and Murlin found that a substance secreted from the pancreas causes hyperglycemia when injected into rabbits and dogs. They decided to name this substance glucagon, short for “glucose agonist3.”
What animal venom contributed to research in GLPs?
Gila monster. In the 1990s, Dr. Eng was researching in how Gila monsters were able to maintain blood sugar despite long periods of not eating, and discovered a peptide called exendin-4 in its venom, this is structurally and functionally similar to GLP14.
Adrenaline vs epinephrine? Acetaminophen vs APAP?
It’s because the English language is derived from so many different roots. Adrenaline derives from Latin, “ad + renal”, or “on kidney”. Epinephrine derives from Greek, “epi + nephros”, which again translates to “on kidney.” The names from Tylenol comes from different abbreviations of its chemical structure.
Acetaminophen = N-acetyl aminophenol.
Paracetamol = N-acetyl-para-acetyl-amino-phenol.
APAP = N-Acetyl-Para-Acetyl-Amino-Phenol.
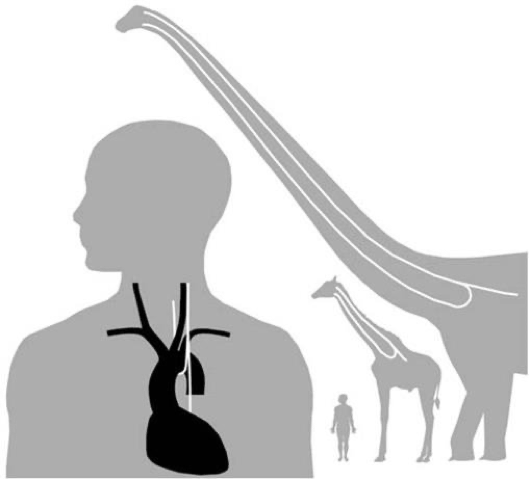
You think you’ve got a lot of (laryngeal) nerve?
The recurrent laryngeal nerve branches from the vagus nerve (CN X) to innervate much of the larynx and control speech. Due to embryological development, the left and right laryngeal nerves wrap around the aortic arch and right subclavian vessels, respectively. As we develop, the heart grows further away from our throat, causing stretching of the “recurrent” nerve. This leads the nerve to make a 10cm U-turn in humans. In Giraffes, the recurrent laryngeal nerve approaches 5 meters. In dinosaurs, this is hypothesized to reach 28 meters5.
Was “War-farin” discovered during research as part of some war effort?
Close, but not quite. Actually, it's not really close either. Warfarin was discovered because of cows randomly bleeding to death. Cattle farmers invited researchers from the University of Wisconsin to figure out why. These researchers discovered that the cattle were eating moldy sweet clover hay, which was found to contain a substance called “coumarin” that anticoagulated the cows and caused them to hemorrhage. The patent rights for this discovery were given to the Wisconsin Alumni Research Foundation (WARF) which is where “WARFarin” originates from, as well as the generic name “Coumadin” from the substance coumarin6,7.
References
1. Zupko RE. Medieval Apothecary Weights and Measures: The Principal Units of England and France. Pharm Hist. 1990;32(2):57-62.
2. Where did the phrase “mad as a hatter” come from? HISTORY. Published May 8, 2023. Accessed January 1, 2024. https://www.history.com/news/where-did-the-phrase-mad-as-a-hatter-come-from
3. Müller TD, Finan B, Bloom SR, et al. Glucagon-like peptide 1 (GLP-1). Mol Metab. 2019;30:72-130. doi:10.1016/j.molmet.2019.09.010
4. Exendin-4: From lizard to laboratory...and beyond. National Institute on Aging. Published July 11, 2012. Accessed January 1, 2024. https://www.nia.nih.gov/news/exendin-4-lizard-laboratory-and-beyond
5. The “Unintelligent Design” of the Recurrent Laryngeal Nerve. Office for Science and Society. Accessed January 1, 2024. https://www.mcgill.ca/oss/article/student-contributors-did-you-know-general-science/unintelligent-design-recurrent-laryngeal-nerve
6. Warfarin Discovery | Wisconsin Alumni Association. Accessed January 1, 2024. https://www.uwalumni.com/news/warfarin/
7. Ankit’s brain. Pharmacy Selective Rotation.