POTD: Dermatology Part 2 Can’t miss diagnoses
This is a continuation of the previous post. There is a lot to learn in the field of dermatology. What are the can’t miss diagnosis that we face in the emergency department?
Red flags of Dermatology
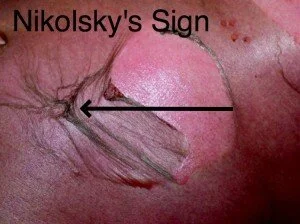
Fever, very young/elderly, toxic-appearing/hypotension, immunocompromised adenopathy, diffuse erythroderma, petechiae/purpura (does the rash blanch with pressure?), nikolsky sign
Nikolsky sign – top layers of skin slip away from lower layers when rubbed
Serious Bullous Diseases
Pemphigus Vulgaris – life threatening (the vulgar one)
Starts in mouth, painful over weeks, non-pruritic, flaccid skin blisters erupt over body, skin breaks easily producing painful erosions (+Nikolsky sign)
Associated with autoimmune disease (myasthenia gravis)
Triggers: captopril, penicillamine, rifampin
Treatment: steroids, IVF, admission to ICU or burn unit, mortality 10-20%
Bullous pemphigoid – not life threatening
Auto-immune disease – mostly in older people, Tense blisters and erosions on skin or mucous membranes
Chronic in older patients, less oral involvement 10-25%, waves and wanes over years, triggered by drugs, UV, radiation therapy
Treat with steroids, consult dermatology
It can be difficult to differentiate bullous pemphigoid and pemphigus vulgaris. The bullae in pemphigus vulgaris are flaccid with possible nikolsky signs as opposed to the tense bullae of bullous pemphgoid. The disease course of bullous pemphigoid is also more chronic, patient often complaining that similar episodes have been occurring for years. There is more oral (90%) involvement of pemphigus vulgaris.
Toxic Shock syndrome
Often secondary to tampon use, abscess, nasal packing, surgical wounds, post-partum
Toxic patient with diffuse erythematous rash that affects mucus membrane and conjunctiva
Acute febrile illness and diffuse desquamating erythroderma, rash will fade in 3 days and will have full thickness desquamation
Steph or strep infection that’s Toxin-mediated, as has superantigens that causes uncontrolled T-cell activation and release of cytokines
Diagnosis: fever, hypotension (SBP<90), rash (diffuse, blanching, macular erythroderma), involvement of 3 organ systems
Rx. Supportive care, IVF, broad spectrum abx, clindamycin for toxin foreign body removal, consider burn unit, IVIG can be used as an adjunct to decease reaction to super antigen
Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
SJS and TEN are part of a spectrum of mucocutaneous reactions often due to medications leading to necrosis and detachment of the epidermis. SJS affects < 10% body surface area. TEN affects > 30% BSA.
Rash: patches often starts centrally, srpeads peripherally sometimes with bullae, can be targetoid, affects mucus membranes including eyes, + nikolsky sign
Triggers: Anticonvulsants, sulmonadmides, NSAIDS, infections
Rx: admit to ICU/burn unit, IVF, supportive care, steroids
Necrotizing Fasciitis
Necrotizing soft tissue infection
Localized not diffuse that may have bullous component, can appear on any body part but most in lower extremities, abdominal wall, perianal/groin regions (Fournier’s)
Treatment: surgical debridement and broad spectrum abx
Diagnosis: gas on XR, low sodium, elevated Cr, crp, glucose wbc, hemoconcentration, LRINEC score