Today I will be discussing the high sensitivity troponin test for diagnosing acute coronary syndrome in the emergency department. Many emergency departments nationwide (and worldwide) have transitioned towards using high-sensitivity troponins. It is crucial to understand the test, benefits compared to standard troponin, use, and interpretation.
High Sensitivity Troponin vs. Standard Troponin for Detection of ACS
High sensitivity troponin recommended by the American College of Cardiology (ACC) in 2022 as gold standard for use in diagnosing ACS in the emergency department. Plethora of evidence demonstrating high sensitivity troponin's ability to detect:
A greater number of MIs within 30 days (without change in mortality rate)
Lower concentrations of troponin compared to standard troponin (mild/subclinical injury)
ACS earlier in course, often 1-3 hours after myocardial injury
Use of High Sensitivity Troponin in the ED
Recommended use in patients with symptoms concerning for ACS in the ED:
Obtain high-sensitivity troponin
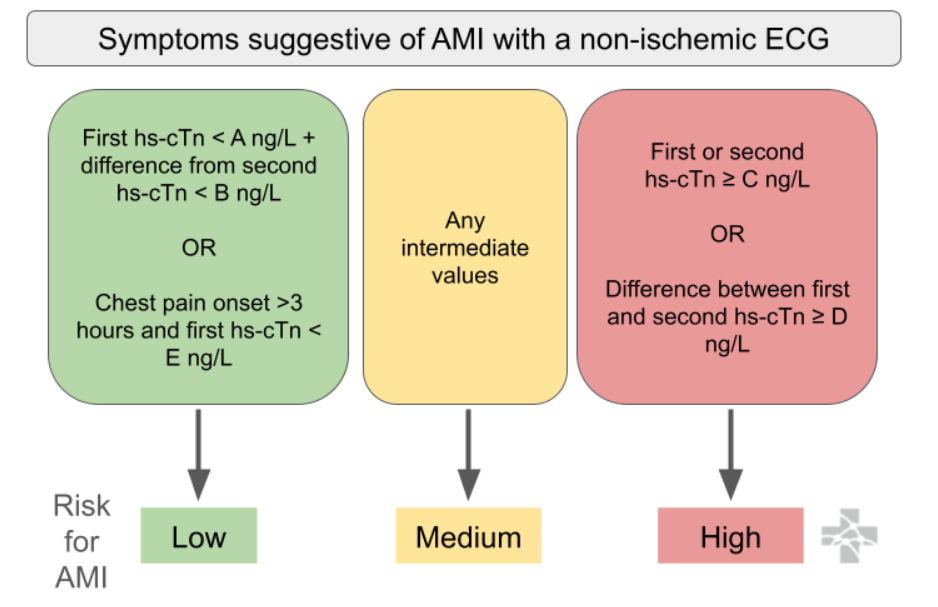
rapid rule-out of ACS with a non-ischemic ECG and either 1) one very low troponin result (depending on onset time of chest pain >3hrs) OR 2) very low change between two consecutive troponins (aka low delta troponin)
Below is an algorithm from Ali-EM for recommended use. Troponins are recommended by the AHA/ACC to be trended every 3 hours, if trending is clinically indicated. Protocols are institution-specific.
Interpretation of High-Sensitivity Troponin
Normal values vary based on type of high sensitivity troponin (institution-specific) and sex:
High Sensitivity Troponin I (hs-TnI) Males: <20 ng/L and Females: <15 ng/L
High Sensitivity Troponin T (hs-TnT) Males: <14 ng/L and Females: <9 ng/L
Limitations
Because high sensitivity troponin tests detect lower troponin levels, there are more likely to be false positives for ACS detection (especially in chronic illness / stress / stable CAD / HF / CKD). This may result in unnecessary testing and invasive measures. Further clinical trials are required to guide clinical-decision making in these situations. Troponins should only be ordered when clinically relevant, and should be carefully interpreted based on clinical context.