Welcome to our exciting Thursday edition of POTD, in which we will be talking about...
PE in pregnancy!
Special thanks to Drs. Hoke and Koch for the inspiration.
We all learn in medical school that pregnancy is a hypercoagulable state, and that these expectant moms are at increased risk of PE and DVT because of this. But to what extent should we be fearing this potentially deadly diagnosis in the pregnant patient who complains of shortness of breath?
The idea that pregnant patients are at higher risk for PE came from epidemiological studies showing a 2-3 fold increase in DVT and PE during pregnancy. However, these studies did not differentiate between DVT and PE, and 2/3 of the cases were actually just DVTs -- does this change your perception?
In a 2015 meta-analysis by Meng et al, only 3 of every 10,000 pregnancies was found to have PE. The actual time of highest risk is POST-delivery, particularly in C-section patients, up to 1 month post-partum.
In a 15 min long EM:RAP segment from March 2016, Dr. Jeff Kline (the PE guru of the EM world) outlines his own reasonable approach to PE workup in our pregnant patients.
1) Start with bilateral lower extremity dopplers looking for DVT
2) If negative, can evaluate the patient using PERC criteria. If the patient PERCs out, discuss with mom either stopping the workup, or continuing on with a D-dimer.
3) Much has been said about trimester-adjusted D-dimer levels. While there are no validated studies on this, Kline proposes cutoffs of 750 ug/mL, 1000 ug/mL, and 1250 ug/mL for the first, second, and third trimesters (assuming an assay with usual cutoffs at 500 ug/mL). I believe our assay cuts off at 380, so not sure how these values figure comparatively...
4) If the D-dimer comes back elevated, the next step is to proceed with pulmonary vascular imaging.
Often, the mom may ask, "What's the actual risk of radiation to my baby?" The real answer is no one can be sure, but here are the fetal doses of radiation from common radiologic studies (from ACOG):
- 2 view plain CXR: 0.0005 to 0.01 mGy (milliGray)
- CT pulmonary angio: 0.01 to 0.66 mGy
- Low dose V/Q scan: 0.1 to 0.6 mGy (perfusion-only scan delivers less radiation, too)
Generally speaking, a fetal radiation exposure of <5 mGy is considered a safe dose in pregnancy.
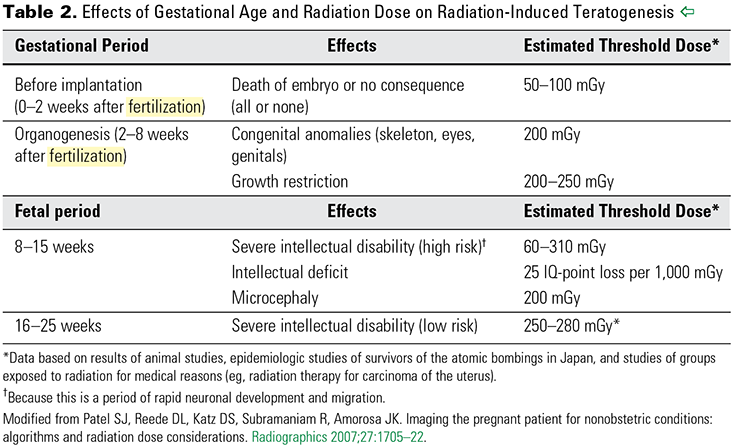
This chart shows the estimated upper limit radiation dose for teratogenic effects, which changes as the fetus develops:
ACOG recommends CT angio over V/Q scan to rule out PE in pregnancy. Why?
- You can see above that a V/Q scan is actually a higher dose of radiation to the fetus. If for whatever reason you cannot get a CT angio, instruct mom to empty her bladder after the V/Q scan is completed, to minimize continued exposure of baby to the tagged radioisotope.
- Next, while CT angio has the added exposure of IV iodinated contrast which can cross the placenta, animal studies have not shown it to have any teratogenic effects.
- Lastly, breastfeeding women have traditionally been told to halt breastfeeding for 24 hr after getting IV iodinated contrast. This is a myth! ACOG states that <1% of iodinated contrast is excreted into the breast milk, and a further <1% of that <1% is actually absorbed through the infant’s gastrointestinal tract. So no real need to pause breastfeeding!
At the end of the day, your clinical gestalt is still key. Also utilize adjunctive tests (bedside echo looking for right heart strain, EKG, CXR) to guide your plan of action.
References:
EM:RAP
