POTD: Pelvic Binder and Pelvic Fractures
TLDR
If there is pelvic tenderness/instability in trauma with significant mechanism or in an unstable trauma patient, a pelvic binder should be placed to tamponade possible massive hemorrhage and assist in stabilizing fractures.
Please watch these short videos on applying a pelvic binder
https://www.youtube.com/watch?v=8dCntKAExBk
https://www.youtube.com/watch?v=Omg79Ced6s0
Today’s pearl of the day covers the use of pelvic binders as well as a general overview of pelvic fractures.
Most pelvic fractures occur due to traumatic, high energy events like a motor vehicle accident. Given its proximity to major organs and blood vessels, they have high morbidity and mortality. (10% mortality for traumatic pelvic fracture, 50% in the unstable patient)
Anatomy
The pelvis is made from the sacrum, coccyx, and the innominate bones (fusion of the ilium, ischium, and pubis). The acetabulum is where the ilium, ischium, and pubic fuse. Pelvic fractures are often classified into acetabular, single bone, and pelvic ring fractures.
Acetabular Fracture
For acetabular fractures, one thing to look for is posterior dislocation of the hip as these need to be reduced within 6 hours of injury. These classically happen when the knee hits the dashboard.
Single Bone Fracture are the most frequently encountered pelvic fractures in the ED and most are stable and are non-operative. For sacral fractures, there is a higher chance for nerve injuries to make sure to complete a full neuro exam.
Pelvic Ring Fracture
These are the most severe fracture type with two breaks in the circular pelvic ring. They have the highest rate of major hemorrhage.
The Young-Burgess Classification system defines three types of pelvic ring fractures
Lateral compression fracture – most common, T bone MVC
Anterior posterior compression fracture – widening of pubic symphysis > 1 cm can represent instability
Vertical shear fracture
Management
If the patient is hemodynamically unstable resuscitate with MTP and give TXA as per normal trauma guidelines
Physical Exam – can rule out significant pelvic injury 93-100% sensitivity in alert patient
Inspect for ecchymosis, deformity, asymmetry, wounds
Palpate for bony tenderness
Compress iliac crest to look for instability; this must be performed gently to minimize hemorrhage if there is a pelvic fracture. Do not rock the pelvis.
If there is a suspected pelvic fracture:
Digital rectal exam for rectal injury i.e. bony fragments, sphincter function, high riding prostate, blood
Genitalia exam – blood at meatus, scrotal, or other hematoma, vaginal exam for vaginal tears
For urethral injuries a RUG (retrograde urethrogram)
For bladder rupture a cystogram
Lower limb length discrepancy and malrotation
Neurologic exam
Pelvic Binder
If there is a pelvic ring fracture, a pelvic binder needs to be placed. This is to decrease the space in the pelvis for hemorrhage and stop active bleed. It also assists in stabilizing fractures.
Pelvic binder should ideally be placed prior to intubation as RSI medications can cause expansion of the pelvic space leading to increased bleeding.
This can be with a commercial binder or with a sheet.
https://www.youtube.com/watch?v=8dCntKAExBk Commercial Binder 78 s
https://www.youtube.com/watch?v=Omg79Ced6s0 Sheet 47s
Studies have shown that sheet binders provide a similar level of stabilization as commercial binders.
Often times, there isn’t time for an XR to identify a pelvic ring fracture. If there is instability on physical exam, pelvic tenderness in an unstable patient, or significant mechanism of injury, a pelvic binder should be placed.
Consideration for not applying a pelvic binder: isolated femoral neck fracture, traumatic hips dislocation, foreign object that would be covered up by the binder
Overall, studies have found that pelvic fractures are very safe and have few complications
Imaging options usually starts with an XR and EFAST.
Given that the patient has a pelvic fracture
In the unstable patient with a positive EFAST, the patient should go directly to OR.
In the unstable patient with a negative EFAST, a diagnostic peritoneal lavage should be performed, if positive, the patient should go to OR.
If both EFAST and DPL are negative, a multidisciplinary team of IR, trauma, and orthopedics should be called to assess if the patient needs angiography with embolization, peritoneal packing, or external fixation.
Once the patient is stabilized, a CT abdomen pelvis with IV contrast, and lastly angiography if an active bleed is found.
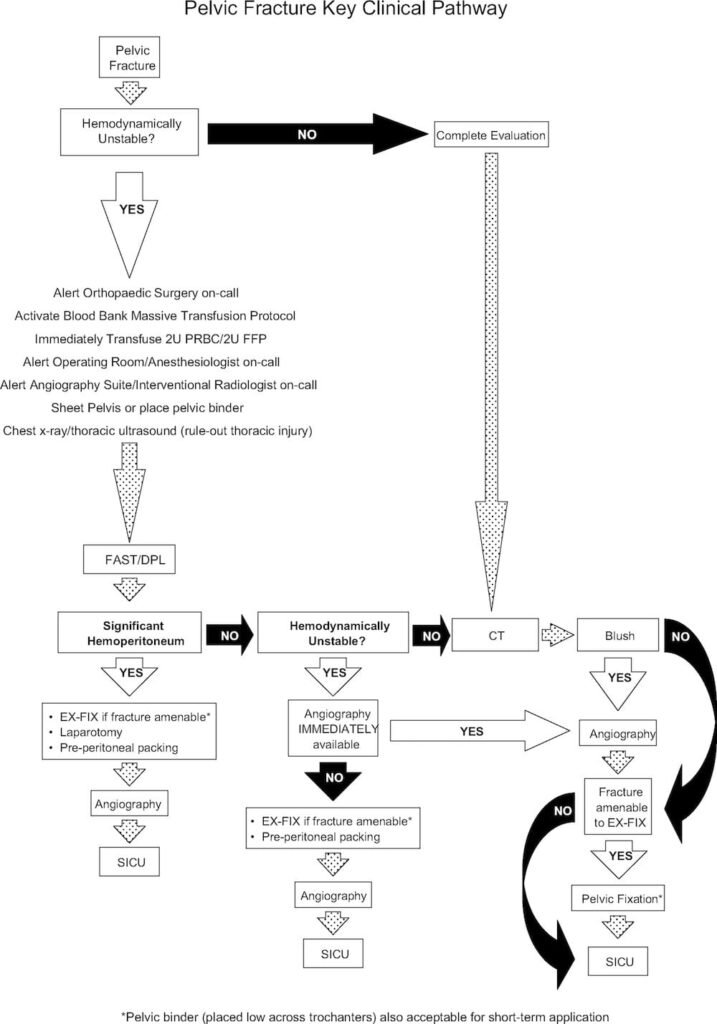
A great flowchart for Pelvic fractures is shown below.