Hey everyone,
After a somewhat heated (well as heated as us third years can get these days) conversation in small group regarding the epistaxis pt with a supra-therapeutic INR I decided to share some info regarding INR reversal based on the current guidelines.
Things to consider:
- Evidence of active bleeding
- Magnitude of INR
- Indicatino for anticoagulation
- RFs for bleeding
- Recent bleed w/in 4 wks, surgery w/in 2 weeks, Plt < 50, Liver disease, antiplatelets
- Volume status?
Options:
- Vitamin K PO and IV- Warfarin is a VitK antagonist so makes sense right?
- Similar affects between PO and IV at 24hrs but IV has onset of 6-8hrs
- FFP- Includes all coagulation factors, has an INR of 1.6
- VitK dependent factors in concentration of 1U/mL
- In a 70 kg Patient: 1 Unit Plasma increases most factors ~2.5% 4 Units Plasma increase most factors ~10%
- PCC (Prothrombin complex concentrate) 3 has Factor 2,9, 10, 4 has 7 also... we only have 4 in our ED I believe.

Bleeding Patient:
- ALWAYS STOP THE COUMADIN!!
- INR >1.5 w/ life threatening bleed ( ICH, GI, hemodynamic instability)
- VitK 5-10mg IV
- PCC 50IU/kg IV AND FFP 150-300mL
- If PCC unavailable then 15mL/kg of FFP
- INR >2 w/ clinically significant but not life threatening bleed
- VitK 5-10mg IV
- PCC 35-50 IU/kg IV
- Minor bleeding:
- Low risk? Rpt INR next day
- High Risk or INR >4.5 PO VitK 1-2mg or IV 0.5-1mg and close followup w/in 24hrs
NOT Bleeding:
- INR <4.5 Omit next dose, resume at lower dose when INR is therapeutic
- 4.5-10: Omit dose
- If High risk bleed consider PO VitK 1-2mg or IV 0.5-1mg and pt needs close followup within 24hrs
- >10: Stop warfarin, VitK, repeat INR at 12-24 hrs
- High risk patient? Consider PCC 15-30IU/kg
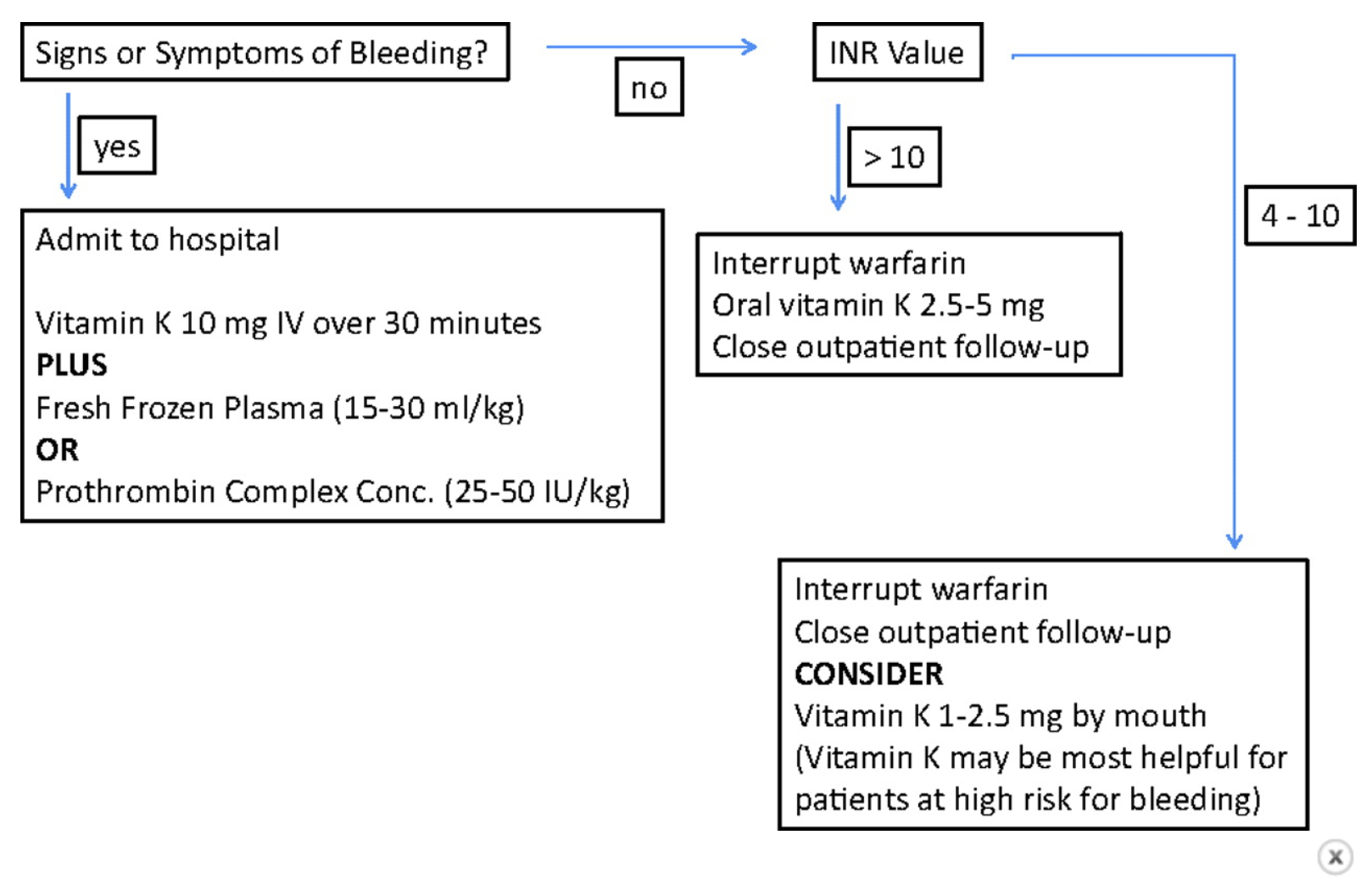
A somewhat simplified algorithm:
A nice concise chart brought to you by our colleagues in Wales:
Sources: Circulation, Surgical Critical Care guidelines, LITFL, CHEST
