This week’s VOTW is brought to you by Dr. Aaron Ryoo!!
17 yom presented to the Bay Ridge (Free-standing) ED with 5 days of right lower extremity pain that started as a scab. Two days later he had an I&D of his right calf by his PMD. Over the day prior to presentation, the patient became febrile with worsening pain and erythema. On exam, he had a large erythematous indurated region along his calf with pain out of proportion to exam and purulent/bloody drainage from the previous I&D site. A POCUS was performed which showed…
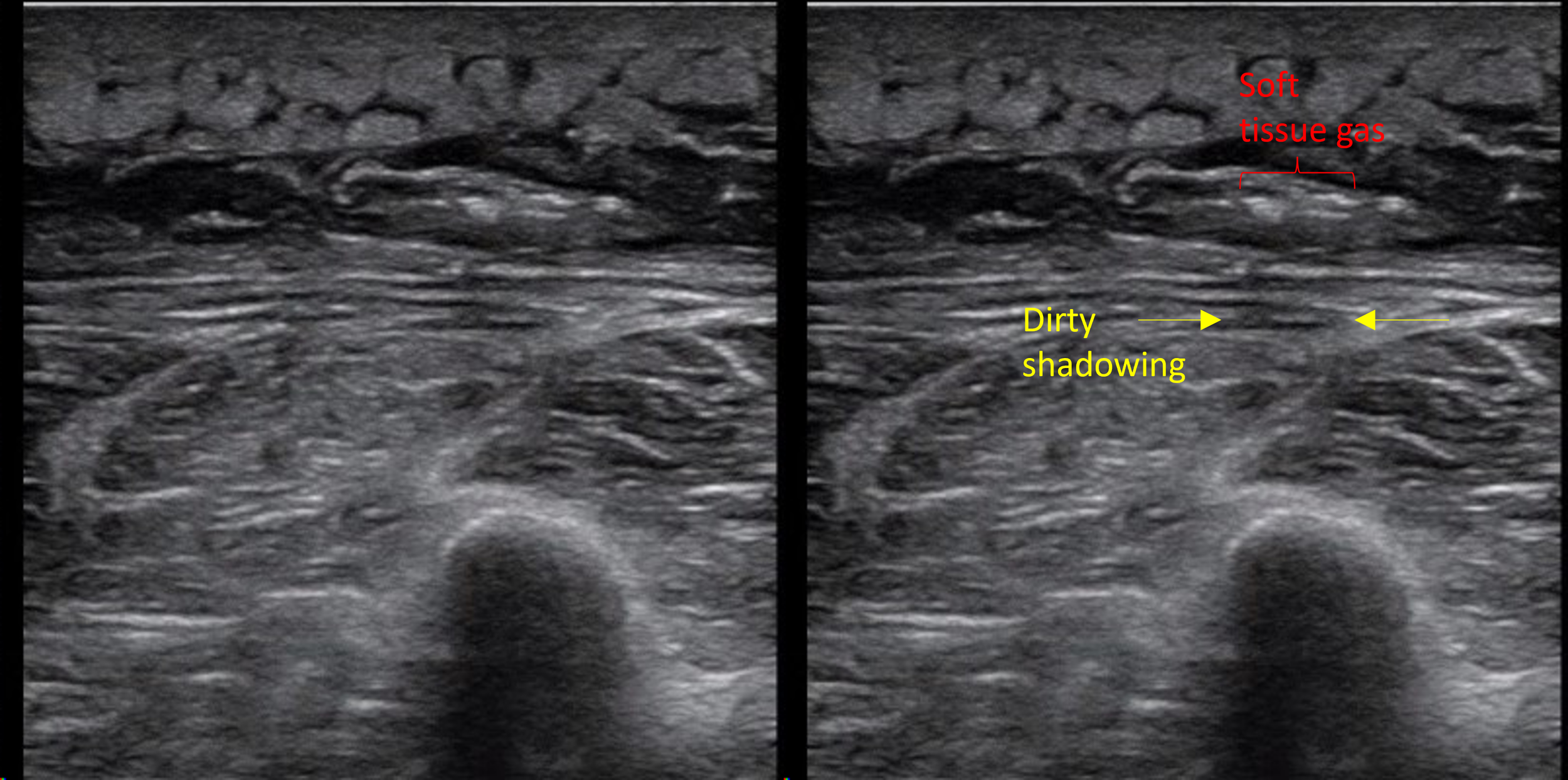
Clip 1 shows a soft tissue image of the calf area, with cobblestoning of the subcutaneous tissues consistent w/ cellulitis. Deep to the subcutaneous tissue there is edema along the muscle/fascial layers and several hyperechoic foci of air with “dirty shadowing” concerning for necrotizing soft tissue infection (NSTI) by gas-forming bacteria.
Necrotizing soft tissue infection
POCUS is a quick and easy way to evaluate for the presence of soft tissue gas when there is a concern for NSTI. Other findings include fluid collections along the fascial plane and findings of overlying cellulitis. Overall, POCUS has a sensitivity of 85-100% and specificity of 44-98% for NSTI1. Fluid accumalation along the fascial planes is most sensitive finding while subcutaneous emphysema is most specific (100%) based on a recent meta-analysis1
You can use the acronym "STAFF" to remember the findings:
ST = subcutaneous thickening
A = air or emphysema
FF = fascial fluid layer greater than 2mm
An I&D can also introduce air into the area but in a septic patient this should be assumed to be necrotizing fasciitis until proven otherwise.
Image 1. Dirty shadowing is caused by sound wave-reflecting objects like gas (think of shadowing from bowel gas). The shadow created is not unformily anechoic. Clean shadowing is caused by sound wave-absorbing objects (think gallstones and bones). The shadow created is unformily anechoic.
Image 1. Dirty shadowing
Findings of cellulitis on POCUS
Skin and subcutaneous tissue appears thickened and diffusely hyperechoic
Area becomes “hazy” with loss of clear borders between epidermis, dermis and hypodermis (subcutaneous tissue)
Cobblestoning- hyperechoic fat lobules in the subcutaneous tissue become separated by edema giving the appearance of cobble stones
Back to the patient:
CT imaging showed “deep perifascial bubbles of gas and edema along the lateral head of the gastrocnemius". Patient was transferred emergently to Maimo and was taken to the OR by general surgery the next morning for an I&D. Purulent material was found along the fascial planes confirming the diagnosis of necrotizing fasciitis.
References:
Marks et al. Ultrasound for the diagnosis of necrotizing fasciitis: A systematic review of the literature, The American Journal of Emergency Medicine, Volume 65, 2023, Pages 31-35
Happy Shadowing,
Your Sono Team