This week's VOTW is brought to you by the ultrasound team starring one of our interns!
A 16 year old male with a history of a previous shoulder dislocation presented to the Peds ED for L shoulder pain after a fall, and was found to have an anterior shoulder dislocation. The UST was paged to the bedside for a interscalene nerve block.
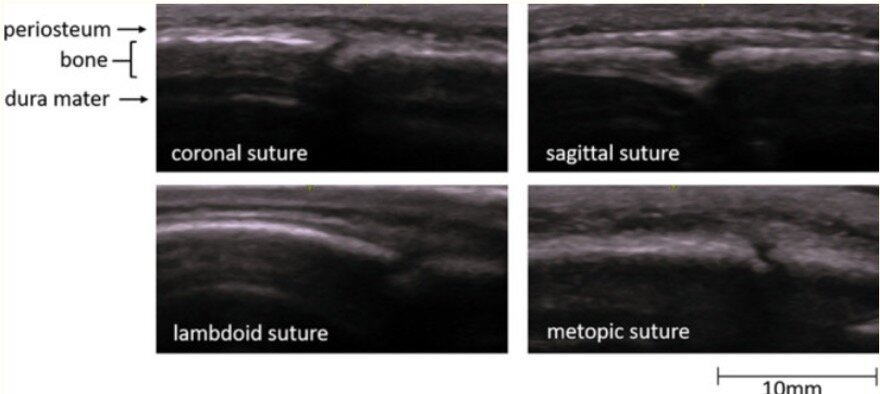
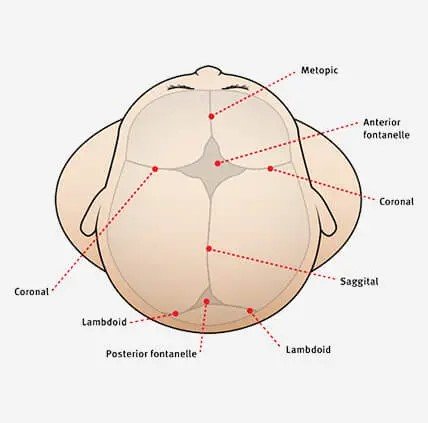
In Image 1 (with probe marker directed medially) we see the anterior scalene muscle, middle scalene muscle and nestled comfortably in between in the interscalene groove is the brachial plexus which has the appearance of a "stoplight". The sternocleidomastoid muscle can also be seen superficial to the anterior scalene muscle. Image 2 shows the same images with relevant anatomy labeled
In Clip 1 we see the needle entering the neck from laterally to medially, using the in-plane approach. Spread of local anesthetic is seen within the interscalene groove. The middle scalene muscle is seen being "pushed" away from the brachial plexus
Dr. Zafrina successfully performed this nerve block and the patient underwent a shoulder reduction using external rotation. The shoulder was reduced within 3-5 seconds w/ minimal effort and the pt said "WOW, that was so much better than my last dislocation!"
Indications of the block
The interscalene nerve block provides blockade to the C5 + C6 + C7 nerve distribution (C8 and T1 are not blocked), and can provide effective analgesia for
proximal humerus fractures
shoulder dislocations
deltoid abscess/I&D
It does not reliably provide analgesia to more distal parts of the arm such as the elbow, nor does it block the axilla. For more distal pathology consider the supraclavicular brachial plexus block or a peripheral block (median/ulnar/radial).
Evidence?
Studies looking at the use of interscalene blocks for shoulder reductions have shown decreased length of stay compared to procedural sedation1 and the block allows us to avoid the complications associated with procedural sedation
This block also provides motor blockade and can make a shoulder reduction significantly easier by relaxing the muscles in the shoulder
Potential complications
Vascular injury- The hypoechoic circular appearance of the C5-C7 nerve roots can look similar to a vessel so use color flow doppler to differentiate it from the surrounding vasculature
Phrenic nerve paralysis- runs along the brachial plexus on the way to the diaphragm. Avoid the procedure in patients with severe lung disease, active respiratory discomfort or a patient with limited lung reserve. Reduce this risk by using low volume of anesthetic (10ml)
As with any nerve block, calculate the max anesthetic dose for the patient, make sure your patient is always on a monitor for quick recognition of the feared complication LAST (local anesthetic systemic toxicity), and know where to find intralipid (above cabinet in resus room 53)
How to perform the block
Get a nerve block kit (cabinet in Resus 54)
Get 5-10ml of local anesthetic
short-acting like lidocaine for a short procedure such as I&D or shoulder reduction
longer-acting like ropivacaine or bupivacaine for a patient going home with a fracture
place patient in lateral decubitus or place a shoulder roll to expose more of the lateral neck region
place a linear probe in transverse orientation at the level of the larynx and identify the carotid and IJ (see image below)
slide the probe laterally to find the sternocleidomastoid, anterior and middle scalene and the brachial plexus- look for the “stoplight”
Using the in-plane approach, direct your needle to the space between the middle scalene muscle and brachial plexus, starting laterally
Inject local anesthetic and watch the middle scalene be pushed off of the brachial plexus
Here is a great resource on how to perform this block from our friends at Highland: https://highlandultrasound.com/interscalene-block
References:
1. Blaivas M, Adhikari S, Lander L. A Prospective Comparison of Procedural Sedation and Ultrasound-guided Interscalene Nerve Block for Shoulder Reduction in the Emergency Department. Acad Emerg Med. 2011;18(9):922-927.
Happy Scanning and Blocking,
Your Sono Team