76 y/o male with no reported PMHx presented via EMS for acute SOB after fall at home. Per EMS, neighbors called EMS after hearing fall as patient lives alone, reportedly admitted recently for a fall in Oct 2025 and declined nursing home upon discharge. EMS found patient to be hypoxic to 70% on RA and improved on CPAP. Patient placed on BiPAP by team with good O2 saturation but decompensated after having an episode of coffee ground emesis on BiPAP with hypotension and abdominal pain. Patient found with diffuse abdominal tenderness and bedside POCUS of the abdomen was completed.
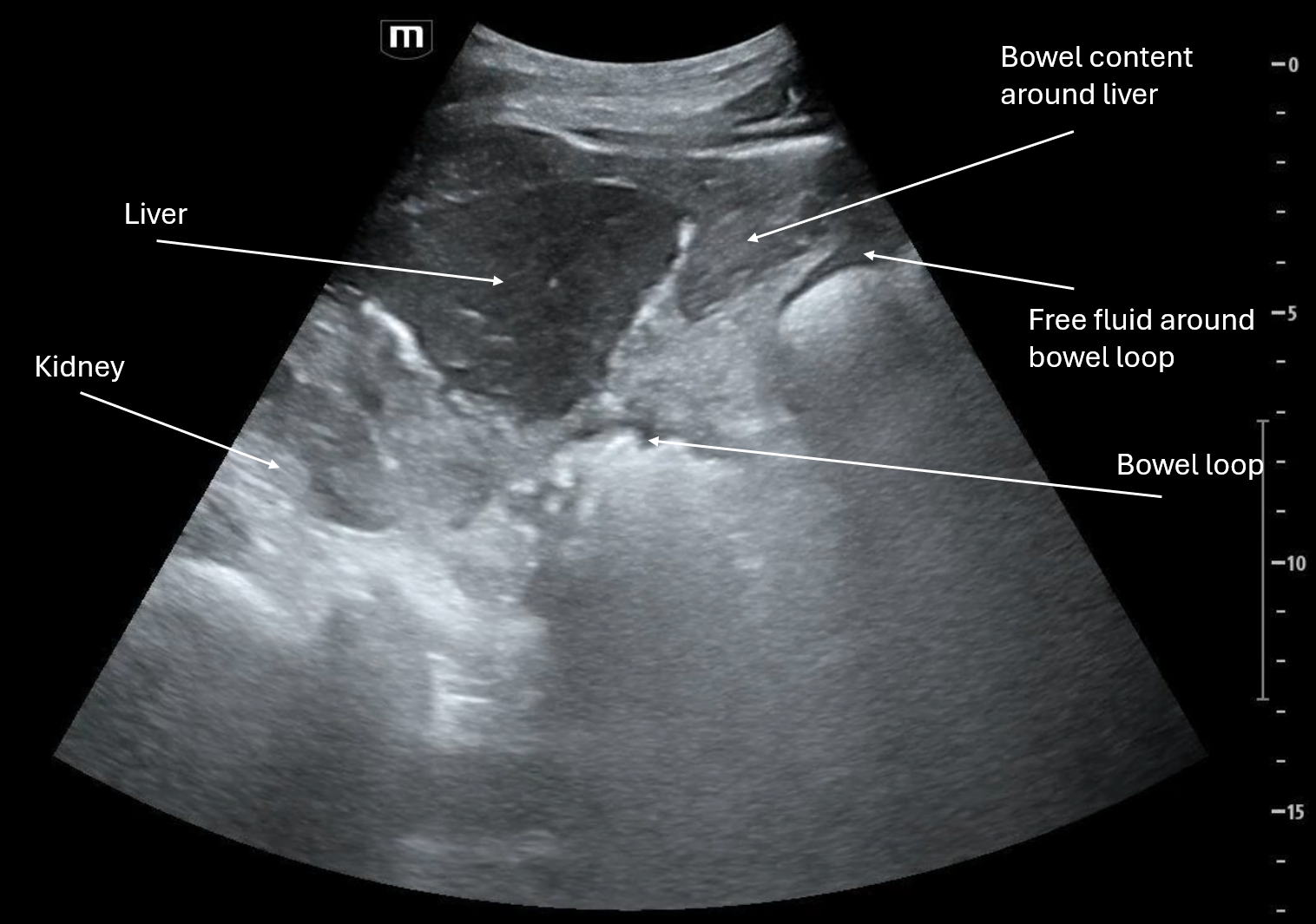
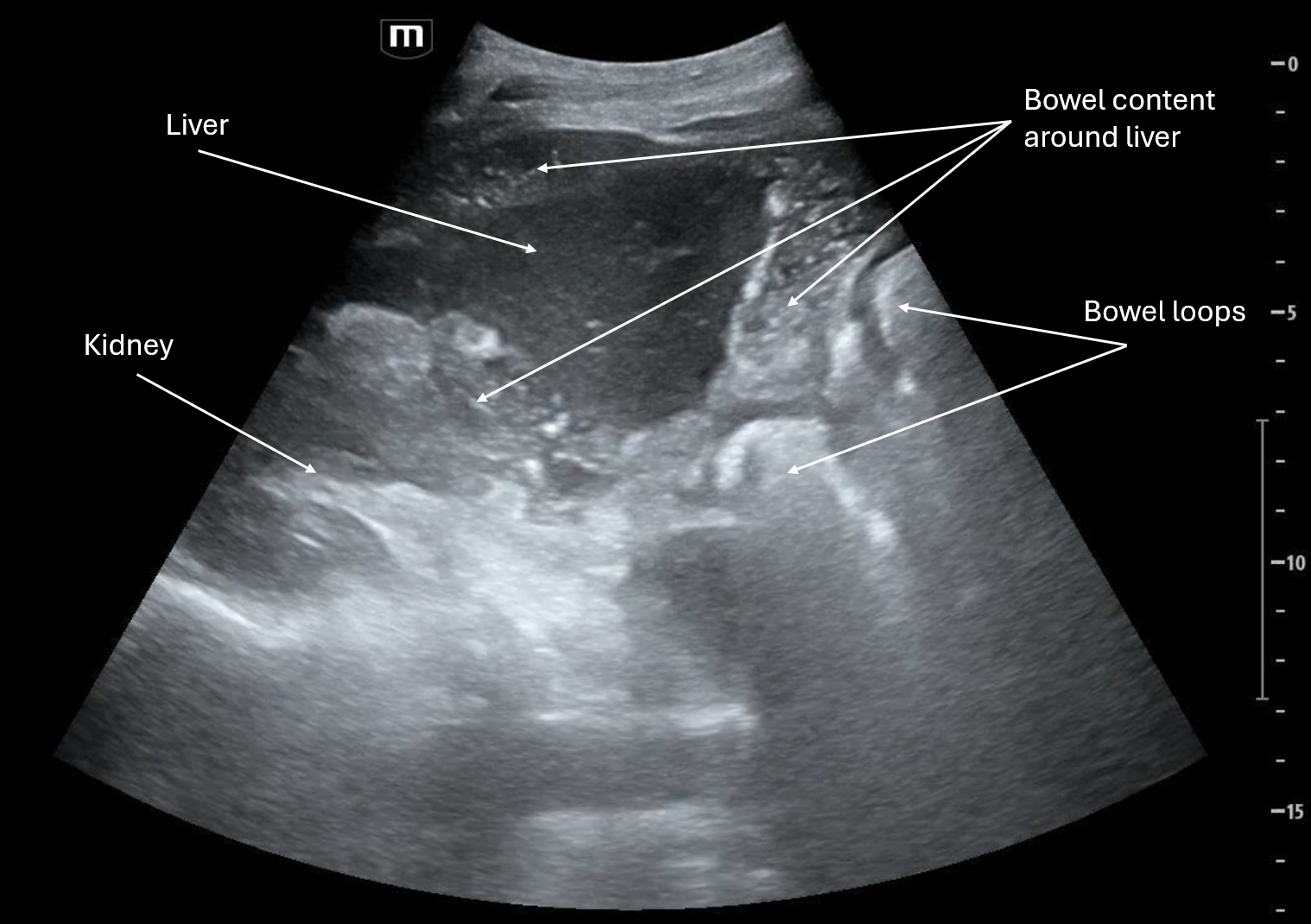
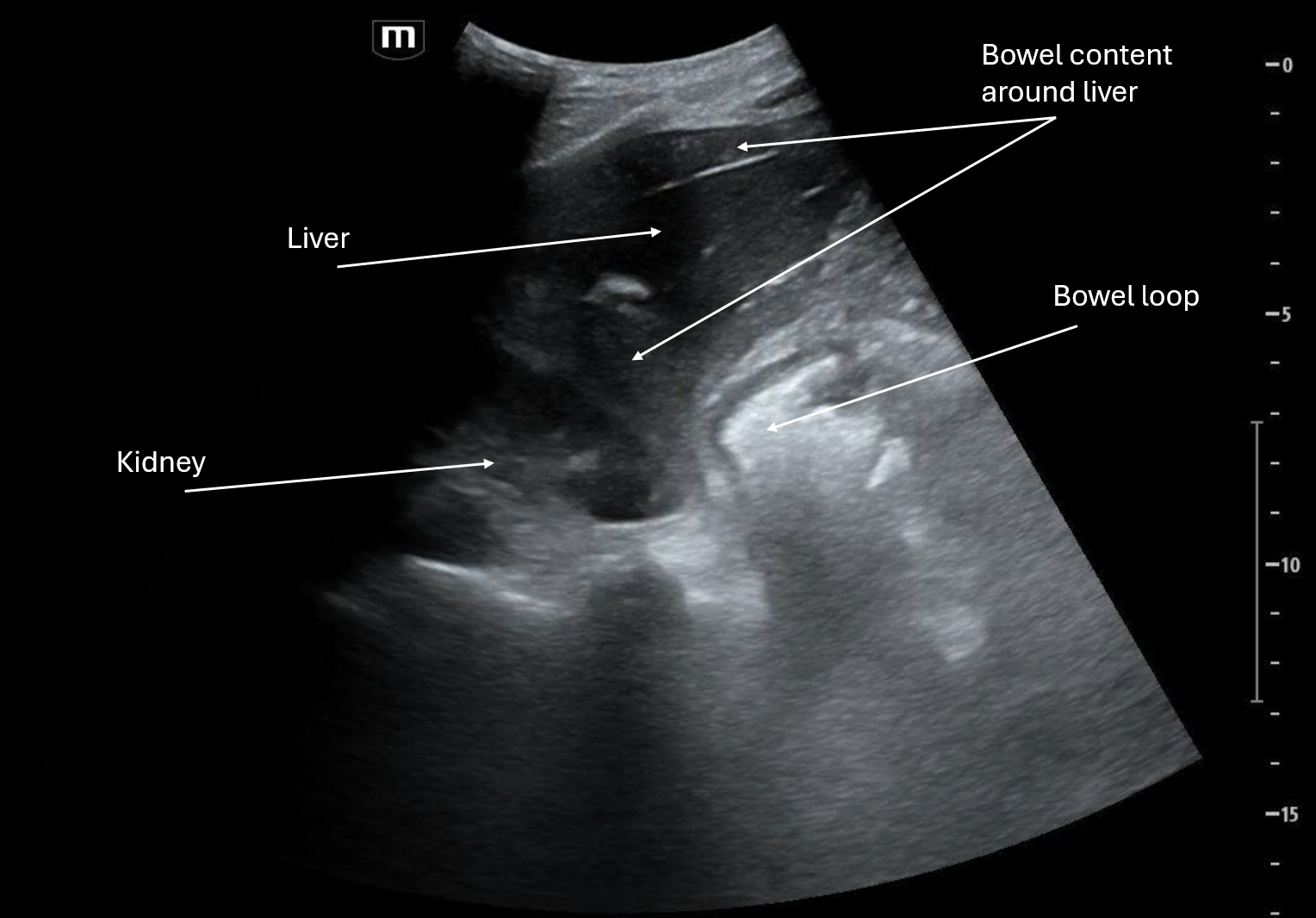
In all 3 clips we see the right upper quadrant, and in different cuts of it you can see that there is some sort of complex fluid surrounding the liver and between the liver and kidney. It isn't anechoic or hypoechoic like we would expect of free fluid like ascites or even blood from an acute bleed, it could be coagulated blood but usually that has more of a layering effect than swirling of hyperechoic and hypoechoic contents.
It may also appear that there is some free fluid around the bowel loops and possibly some bowel wall edema which all points to perforated bowel and resulting global bowel inflammation.
Patient was unstable and due to episode of coffee ground emesis was presumed to be GI bleed with perforated viscus. Patient was taken emergently to the OR without a CT scan and they found "large volume feculent peritonitis, global intraabdominal necrosis (SB, colon, stomach, liver, diaphragm, peritoneum), 1cm cecal perforation." Patient's prognosis was grave and died several hours after the OR.
We are very sorry for his family's loss and respectfully thank him for this learning opportunity.
POCUS Pearls
Free blood
Anechoic to hypoechoic when acute
Becomes heterogeneous / mildly echogenic as it clots
Usually smooth, homogeneous, without internal architecture
Stool / bowel contents
Heterogeneous, mixed echogenicity
Often dirty shadowing
May have mottled, granular appearance
Can show gas with reverberation or ring-down appearance