Hello all! This week’s VOTW is brought to you by myself.
Hospital course
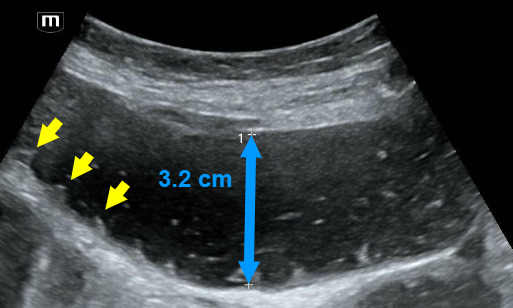
50 y/o F presents to the ED with several weeks of lower back and left knee pain. Left knee is swollen and tender with palpation. She limps when ambulating due to the pain. Bedside ultrasound of the knee joint is shown below.
In the image above, the probe is placed over the suprapatellar space with a long-axis view. The femur is seen below, with a layer of dark anechoic effusion visible between the quadriceps tendon and the prefemoral fat pad.
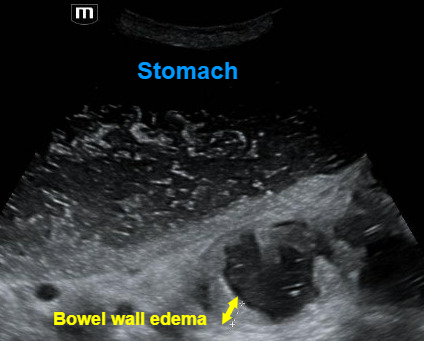
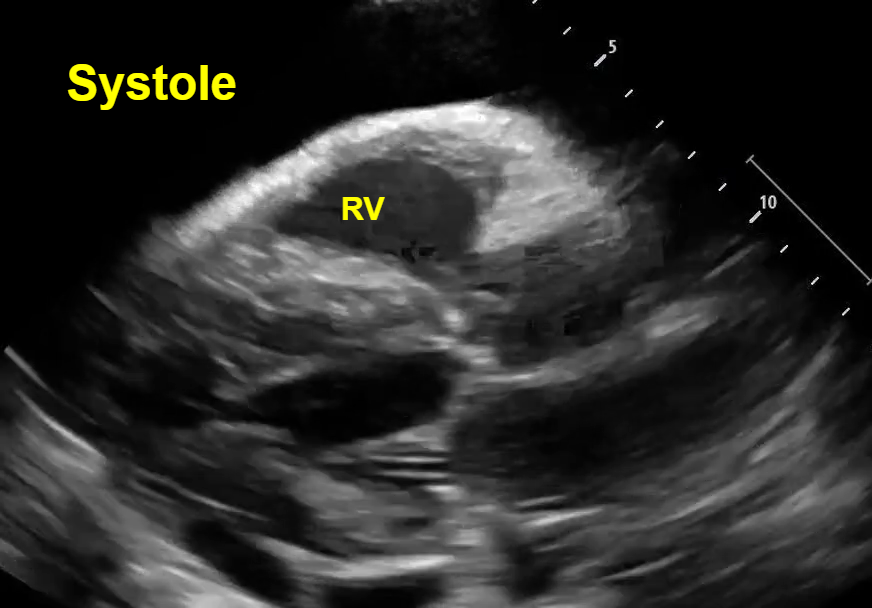
Once the suprapatellar effusion was identified, the probe was rotated 90° into a transverse view of the knee, and the needle was inserted lateral to medial using an in-place approach. In the image above you can see the needle tip enter the effusion underneath the quadriceps tendon. The needle is the hyperechoic straight line in the left image, which is labelled with a white arrow in the right image.
In the clip above we can see this ultrasound-guided in-plane needle insertion with the needle tip entering the suprapatellar effusion.
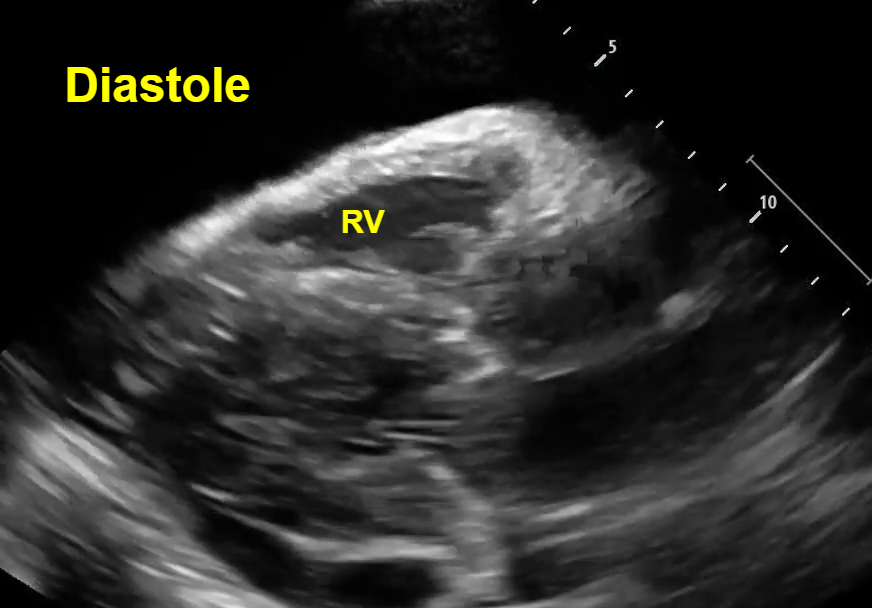
In this clip, we can see the effusion shrink in size as the synovial fluid is actively aspirated through the needle!
Case Conclusion
The synovial fluid specimen was sent to the lab, and septic arthritis was ruled out. The patient’s left knee pain significantly improved after the arthrocentesis and she was discharged.
Ultrasound-guided knee arthrocentesis
· While this procedure can be performed blind, the use of ultrasound improves accuracy, improves pain scores, and allows aspiration of more synovial fluid.
· The patient should be positioned supine with the knee in 15-20° of flexion.
· Begin by identifying a suprapatellar effusion by placing the linear probe superior to the patella with the marker oriented cephalad (long axis view of the knee). A joint effusion will look like an anechoic stripe within the joint space deep to the quadriceps tendon.
· Once you identify a drainable effusion, rotate the probe 90° to obtain a transverse view (short axis view of the knee). A lateral to medial in-plane technique should be used to guide the needle tip into the joint effusion.
· Remember to use a sterile ultrasound probe cover!
· Ultrasound-guided arthrocentesis can be used to drain effusions from any joint, with commonly aspirated joints including knees, hips, shoulders, wrists, elbows, and ankles.
Happy scanning!
Sono team
Resources to review:
· https://www.acep.org/sonoguide/procedures/arthrocentesis